My last two blogposts looked at safety culture and organisational learning. I argued in my first blog that in the healthcare sector, there is strong evidence that having a positive culture of safety was associated with better outcomes for patients. In my second post, I presented the idea of organisational maturity in learning and covered Westrum’s maturity model as well as the expansion of the model to create MaPSaF, the Manchester Patient Safety Framework.
At HRA, we have found that reporting culture – an essential element of safety culture – isn’t quite as healthy as we might hope, both in healthcare and other industries. It’s still often seen as a bureaucratic process, carried out with good intentions but frequently ignoring contextual factors in incidents, too often focused on blame.
In this post, I want to turn our spotlight on culture and systems in pharma manufacturing and take a look at corrective and preventive action or “CAPA”.
Do systems rule – or does culture eat them for breakfast?
OK – this is a provocative phrase but useful. I believe that culture can certainly over-ride systems and lead, for example, to the normalisation of sometimes unsafe practices. But then, systems set the structure, policy and practice. So, which is dominant? Neither, of course – they are each an element in organisational behaviour and their interaction is inevitable. An organisation may have an excellent reporting system, for example, user-friendly and responsive, focused on learning and so on – but reporting may be effectively disabled if staff do not feel they will be treated fairly by managers.
Both systems and culture will be important wherever a process is designed by and managed by people, as in pharmaceutical manufacturing.
What is CAPA?
CAPA comprises:
- “corrective” actions in response to quality/safety problems in pharmaceutical manufacturing and medical devices, defined as the elimination of the cause(s) of non-conformity to prevent recurrence, and
- “preventative” actions designed to eliminate the causes of potential non-conformity1.
In general, it’s probably fair to say that the first of these predominates and that companies must be able to demonstrate their response to deviations identified by regulators. However, I will argue that a human factors-based approach to deal with CAPA management has significant benefits for the sector.
CAPA management – a model system
The overall system in place to address CAPAs is modelled below in figure 1.
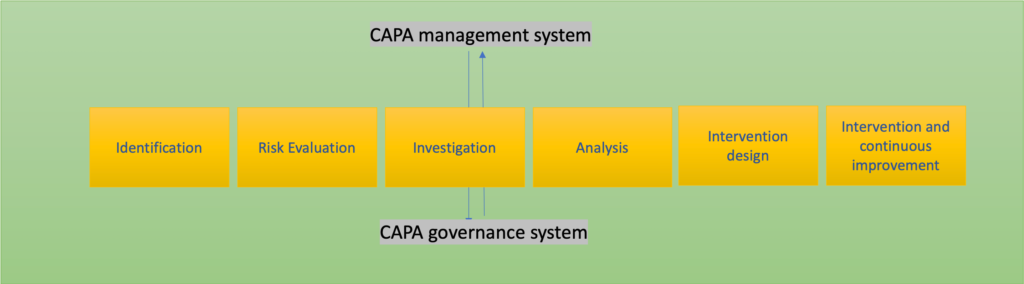
This model, which reflects industry good practice2 sets out a sequence of actions, together with the requirement for an overall governance process. How can a Human Factors approach, including having a positive culture, support these steps?
Step 1 – identification
Most CAPAs represent a reaction to deviations identified by either regulators or internal quality systems. This reactive approach is essential, of course, for safety and productivity – but there is another, less painful, way to deal with risk, after all: proactively.
“Preventative” in the CAPA definition is often seen as making sure that a detected problem does not recur. In human factors, however, we place a great emphasis on averting problems which have not yet arisen through proactive risk methodologies. Of these, the most important is Safety Critical Task Analysis (SCTA), where a high-risk process is analysed for potential failure, including human contributions to failure, and the system refined or redesigned as a result. Using SCTA systematically to screen processes and systems has been shown to reduce risk before problems manifest themselves in costly and unsafe ways.
Step 2 – risk evaluation
A systematic risk evaluation, usually based on a detailed task analysis developed by safety and process engineers but – critically – with the frontline staff involved throughout, will help to identify high-risk or vulnerable steps. In addition, a risk analysis will enable a ranking so that highest risk elements can be addressed first, and may also enable grouping of CAPAS and a more efficient approach to managing deviations. In case where human error is a factor, for example, we may find common contributing factors or performance influencing factors that bear on several potential deviations.
Step 3 – investigation
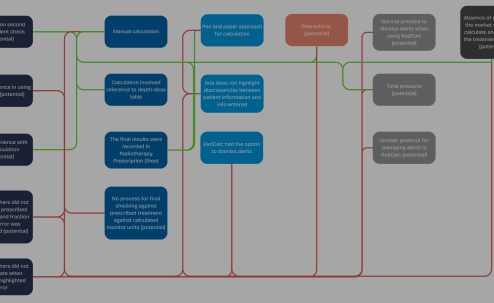
Here, it is essential to take a systems-based approach, and to recognise that a single “root cause” is a very rare event. More important is to investigate the system and look for contextual factors that create the ground and potential for mistakes. In this model, human error is seen as a consequence, not a cause (though there may be exceptions). Investigations should focus on risk throughout. What are the risk control measures? What risks are not adequately controlled?
Step 4 – analysis
The essential analytical phase must include risk, as above, and must examine the potential for human error and performance influencing factors. Some of these will be unique to a particular process and some will be general and affect performance in many areas – factors such as distractions, communication, environmental noise, temperature etc. – and culture, of course; see below!
Step 5 – intervention design
We know that human error is a major factor in deviations – ICH (Q9)3 in particular refers to “operational design that is vulnerable to human error”, for example. Fixing the system needs a great deal more than an exhortation to work more carefully, or the application of disciplinary systems. Starting with the perspective that nobody comes to work to do a bad job, we emphasise the following essentials in intervention design:
- adopt a consensus approach – involve and respect operational staff and their direct experience
- make risk evaluation and knowledge of the residual risk a priority throughout the intervention design process
- use the Hierarchy of Control intelligently to rank the likely effectiveness of the proposed interventions (note that “training” is usually considered as having low effectiveness compared to other interventions)
- make sure that we use meaningful metrics and that balancing metrics are also included – new risks may be created by the interventions.
Step 6 – intervention and continuous improvement
Here, interpretation of metrics is needed as part of the overall governance programme of measurement and monitoring. Finding ways of sharing experience and responding to problems is essential, as is the continued involvement of frontline staff.
… and culture?
Once again, the significance of culture cannot be ignored. A company may have a solid system in place to manage CAPA and develop quality, but… what if staff respond unfavourably to the statements below, for example?
- Staff here generally do not know about outstanding or uncontrolled risks
- At this site, we usually assume that everything is going well and only make changes after an incident
- We only address major CAPAs or deficiencies identified by regulators
- Investigations here are mostly about completing the paperwork
- Most members of staff here feel that investigations are looking for who to blame
- Once we have identified the action that directly caused the problem, we stop looking further
NB: These statements are part of HRA’s CAPA Culture evaluation instrument
… or any of many other beliefs, values or behaviours influence the local culture adversely.
The cultural issues in managing CAPAs are significant and not yet well understood. Working with quality experts from pharmaceutical manufacturing, device design, human factors and organisational learning culture, HRA has developed a methodology to measure and describe “CAPA culture” and address the questions above and many more.
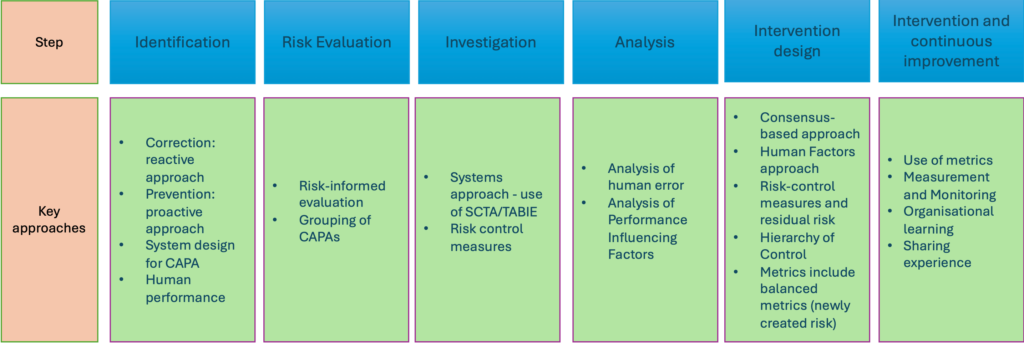
Main approaches we recommend for ensuring a robust CAPA system and develop a CAPA Culture are shown below in Figure 2.
We are seeking partners from the pharmaceutical and medical device industries to work with us in refining and evaluating our approach to CAPA culture and CAPA management. If you would like to be part of this new and exciting work and would like a chat to explore it, please
email Steve Cross at [email protected]
HRA will be launching a new course called SYSTEMS Critical Task Analysis to support industries like pharmaceutical manufacturing in improving safety and quality. More information on the course can be found here: SYSTEMS Critical Task Analysis (SCTA) Course (humanreliabilityacademy.com)
References
- Vantrieste, M. and Amgen, S. (2011). CAPA within the Pharmaceutical Quality System 1. [online] Available at: https://www.fda.gov/media/85266/download.
- Koziol, D. (2020). What Is CAPA in Pharma? [online] PTC. Available at: https://www.ptc.com/en/blogs/plm/what-is-capa-in-pharma
- Food and Drug Administration (2021). ICH Q9 Quality Risk Management – Scientific Guideline. [online] Available at: https://www.fda.gov/media/159218/download.